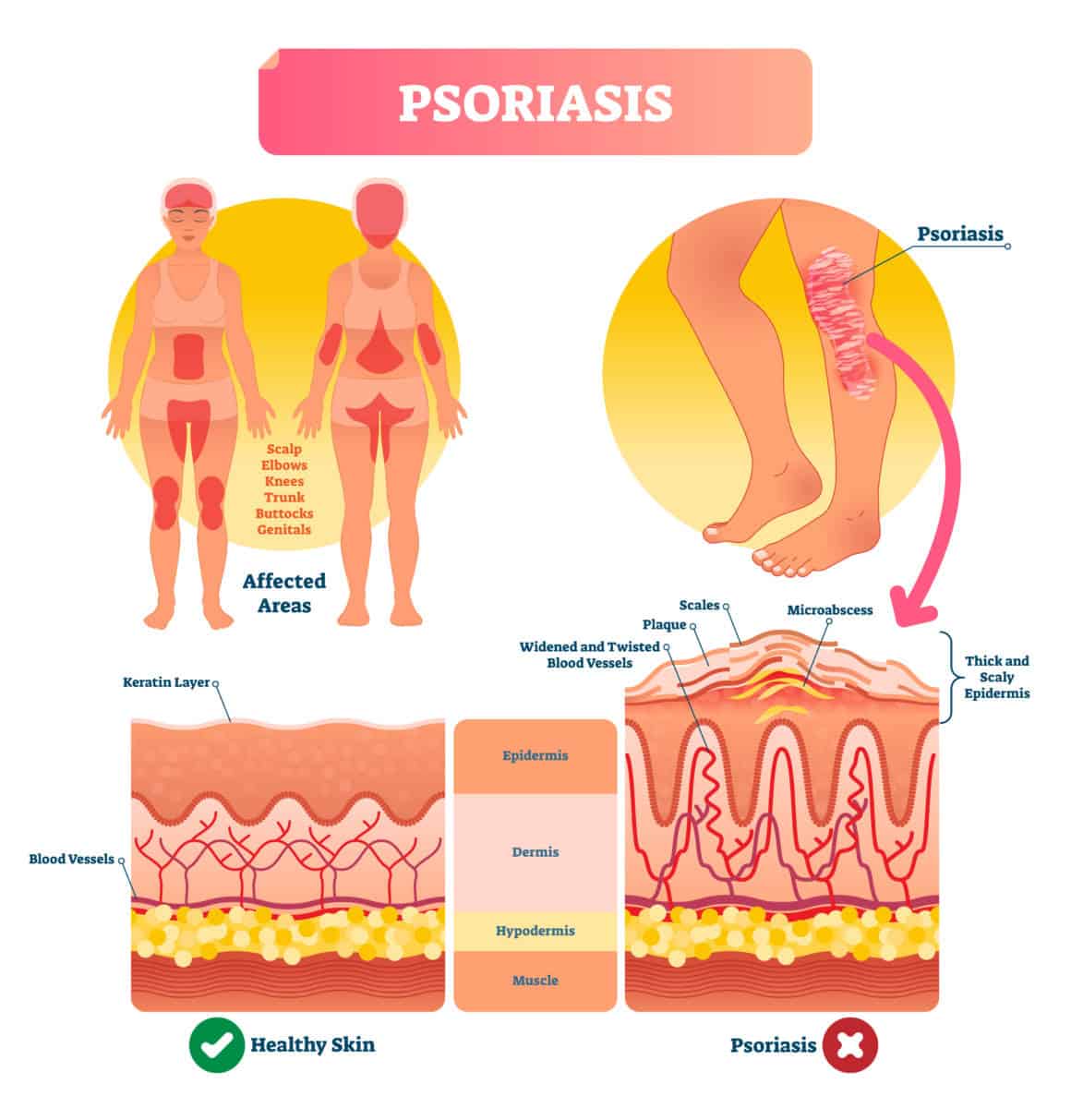
Scientists are not sure what the exact cause of psoriasis is; however, it is clear that genetics and the immune system play a significant part in its development. Internal swelling may be the specific cause of the symptoms experienced with psoriasis, including the red, itchy patches that develop on the skin.
The Role of White Blood Cells
White blood cells (T-cells) are part of the immune system. These cells attack viruses and bacteria, which helps prevent sickness. However, when something with the immune system goes awry, an immune-mediated inflammatory disease (IMID) (autoimmune disease) can result. In other words, the immune system can malfunction. Since psoriasis occurs when the immune system’s T-cells mistakenly begin attacking the body’s own natural skin cells, this disease is classified as an immune-mediated inflammatory disease (IMID).
As the T-cells are attacking the skin cells, the body begins creating new skin cells more frequently (about seven times faster than normal). Unfortunately, the body is unable to shed these additional skin cells quickly enough, which is why they build up on top of the skin’s surface, resulting in the look that characterizes psoriasis.
Unfortunately, once the T-cells consider skin cells as intruders, this misidentification tends to continue for the remainder of the individual’s life. However, the one exception to this rule is guttate psoriasis; some children who develop this form of the disease only have the symptoms once.
Causes and Risk Factors
Genetics
Psoriasis is a genetic autoimmune disease, with up to 10 percent of individuals inheriting at least one of the genes known to be connected to psoriasis. Of this 10 percent, only 2 or 3 percent will develop the disease.
If one parent has the genes for psoriasis, the child’s likelihood of developing the disease is 10 percent. When both parents have the genes for psoriasis, that risk increases to 50 percent.
Other Risk Factors
If an individual has inherited the genes to develop psoriasis, the following risk factors could trigger its onset:
- Skin trauma: Bruises, scratches, and bumps can cause the immune system to overreact, resulting in the onset of the condition or a subsequent flare-up.
- Metabolic syndrome: This term refers to a group of conditions that frequently occur collectively, which includes obesity, hypertension, type 2 diabetes, and heart disease.
- Infections (strep throat, tonsillitis, bronchitis, etc.): The immune system fights infection; however, when this system is overactive, faulty signals trigger inflammation. The problem results when the inflammation continues despite the infection being cleared.
FAQ
Can psoriasis go away?
The only form of psoriasis that may go away is guttate. Although psoriasis cannot be cured, it can go into remission. Better yet, today there are numerous treatment options available to manage the disease.
What foods trigger psoriasis?
According to a 2018 review, diet can play a role in managing psoriasis. The foods that trigger psoriasis flare-ups, though, can differ from one person to the next. Determining which food will trigger a flare can be accomplished by singling out each food group and then noting if symptoms are experienced; a food diary can help with this task.
That being said, common triggers include:
- sugar,
- vegetable oils,
- seed oils,
- high fructose corn syrup,
- refined carbohydrates,
- alcohol, and
- artificial trans fat.
People who have psoriasis can help manage their disease by consuming foods that are known to reduce inflammation. Medical News Today suggests that individuals with chronic inflammation try the DASH or Mediterranean diet because these diets include many of the foods known to reduce inflammation. These foods include fish, vegetables, fresh fruits, whole grains and healthy fats.
Is psoriasis brought on by stress?
Yes. According to some reports, stress may be a trigger for up to 68 percent of adults with psoriasis. Stress can trigger inflammation, which is why it can cause a flare-up. Therefore, avoiding stressful situations as well as reducing day-to-day stress through meditation and/or practicing yoga (or other stress-reduction practices) can help prevent a flare-up.
Disclaimer: this article does not constitute or replace medical advice. If you have an emergency or a serious medical question, please contact a medical professional or call 911 immediately. To see our full medical disclaimer, visit our Terms of Use page.