Fibromyalgia, or fibrositis, affects up to 6% of the world, according to the National Fibromyalgia Association. In the United States, approximately 10 million people suffer from this condition. Despite how common (and exhausting) it can be, fibromyalgia is fairly controversial. At the heart of this controversy is the question: Is fibromyalgia real?
What is Fibromyalgia?
Fibromyalgia is a condition characterized by widespread body pain. Often accompanying the pain are other symptoms like fatigue, sleeping problems, and mental health issues like depression. What’s more, experts estimate that this condition costs the United States up to $14 billion every single year. To put these numbers into perspective, that amounts to a national productivity loss of up to 2%.
Clearly, the physical, emotional, and financial costs of this condition cannot be understated.
Why, then, do people think this disease doesn’t exist?
Lack of Objective Diagnostics
There are a few reasons.
The largest, though? There aren’t objective diagnostic measures for this condition. Specifically, there aren’t any biomarkers that indicate that there is anything physically wrong with someone. In other words, there are no blood tests, MRIs, or other sorts of exams with quantifiable data that can identify fibrositis.
For example, doctors can use blood work, biopsies, and scans to detect cancer. With fibromyalgia? No such diagnostic tests exists. Since there currently exists no objective way to quantify fibrositis, many peopleâincluding healthcare professionalsâdismiss patients’ complaints.
Physicians’ Disbelief of Patients
Other arguments against fibromyalgia include the notions that patients are over-exaggerating their symptoms or simply making them up all together. The fact that the majority of chronic pain patients are cisgender women could play a part in this response. Firstly, some research shows that cisgender women may feel pain more intensely and for longer periods of time than cisgender men do. Secondly, there is no shortage of research showing that medical bias against cisgender women is real.
So, what happens when coupling a greater propensity to feel pain with a medical provider more likely to disbelieve the average patient? More than likely, it creates a perfect storm for skepticism of not just fibrositis, but other chronic pain conditions, too.
What are the Symptoms of Fibromyalgia?
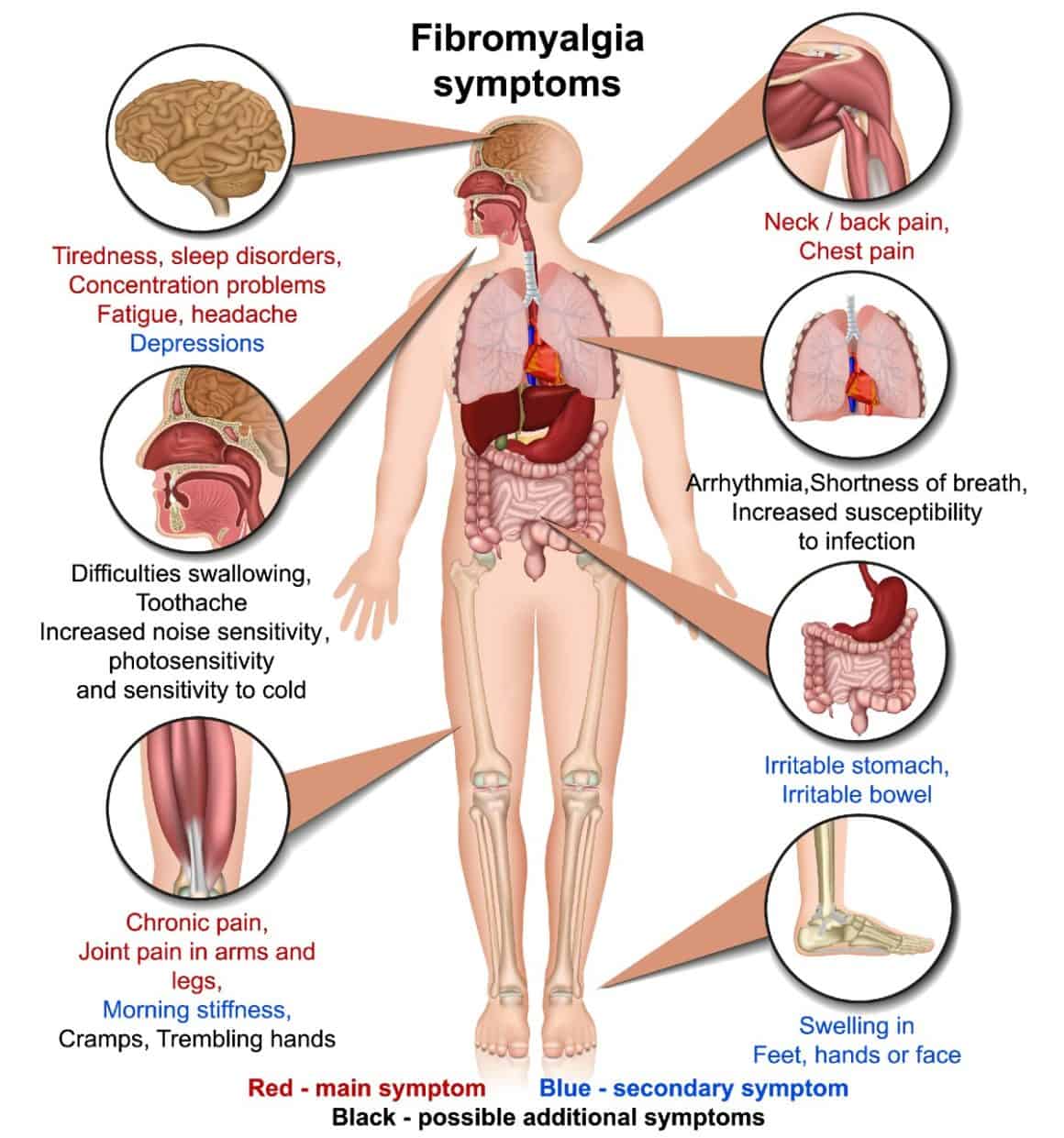
Widespread pain is the hallmark of this condition. What does the pain feel like, though? Some describe it as being like “pins and needles” or even burning. Others still describe it as heightened sensitivity to pain. This pain tends to localize in specific spots in the body.
As mentioned before, fatigue, sleeping problems, and depression are also common symptoms. They aren’t the only ones, however. According to the National Fibromyalgia Association, other signs of fibrositis include:
- Anxiety
- Difficulty concentrating
- Dizziness
- Upset stomach
- Irritable bladder
- Restless leg syndrome (RLS)
- Light sensitivity (photophobia)
- Sensitivity to sound
- Sensitivity to touch
- Headaches
How Does a Person Get Fibromyalgia?
Experts currently don’t know what causes someone to develop this condition. That being said, the following are probable risk factors for fibromyalgia, according to the CDC:
- Age: Odds of developing this condition increase with age.
- Other conditions: Specifically, lupus, rheumatoid arthritis, or similar diseases increase risk.
- Heredity: Those with a family history of the condition are more likely to develop it themselves.
- Sex: Cisgender women are about two times as likely as cisgender men to develop the condition.
- Repetitive injuries: Repeated injuries, particularly on a joint, can increase risk.
(Note that this is not a complete list.)
How is Fibromyalgia Diagnosed?
As mentioned earlier, there aren’t any objective tests for this condition. So, how in the world do doctors diagnose fibromyalgia, anyway? Diagnosis typically involves a combination of the following:
- Ruling out other possible causes of pain through the likes of blood tests and MRIs;
- Physically examining the patient; and
- Reviewing a patient’s health history, including family history.
How Serious is Fibromyalgia?
Many people manage fibrositis after they receive a proper diagnosis and, subsequently, proper treatment. Treatment for this condition includes:
- Medications
- Cognitive behavioral therapy (CBT)
- Exercise
- Stress management
- Good sleep hygiene
Unfortunately, not receiving treatment increases the risk of complications, which include:
- Increased rates of depression;
- Increased risk of suicide and injury; and
- Lower quality of life.
(Note that this is not a complete list.)
Final Thoughts: Is Fibromyalgia Real?
Yes, fibromyalgia is a real condition, although a frustrating one since experts know so little about it. Fortunately, many people manage their health properly, after receiving a proper diagnosis. Therefore, those who believe they may have this condition should discuss their concerns with a healthcare provider. It’s important this provider is someone they can trust to take these concerns seriously.